THE PROBLEM
Traumatic brain injury (TBI) is one of the most complex brain disorders to understand, and one of the most difficult to treat. Military personnel sustain TBIs more frequently than the general population from deployment and from training. Even mild TBIs or concussions can lead to chronic cognitive issues. More severe TBI may lead to long term neurologic impairment. All TBI increases the risk of later neurodegenerative diseases. Our current treatments are aimed at addressing the symptoms of brain injury, as we are not able to correct or repair the underlying deficits. In order to develop treatments for TBI we need to unravel the complex cascade of events that occur at different times after the initial impact. We will then be able to target specific processes to halt, reverse or repair the progression of harmful events.
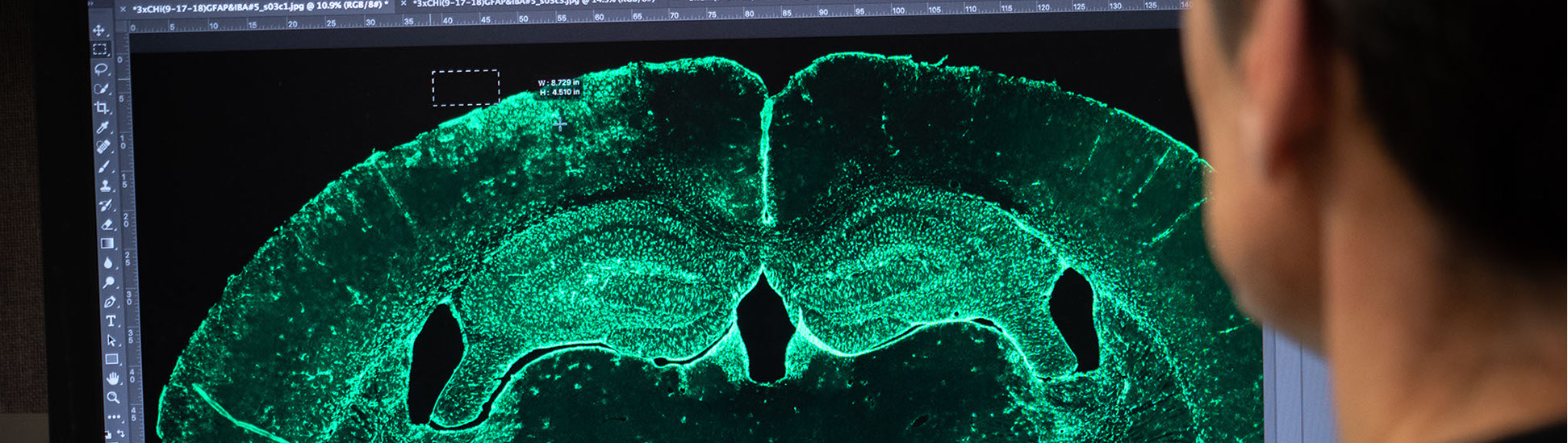
OUR APPROACH
We focus on understanding the molecular signaling cascades that occur after TBI in addition to testing potential therapeutics to enhance recovery from injury. We currently utilize several different rodent models of traumatic brain injury (TBI), and determine functional outcomes after different treatments with behavioral assays that measure movement, memory, anxiety and awareness. We correlate behavior with changes in the cellular and molecular profile of different brain regions to fully assess the effects of the manipulations. In this way we are beginning to understand the complex interactions that occur after injury, and determine how targeted therapeutics impact functional recovery. We also utilize primary cell cultures to tease apart the molecular signaling pathways that contribute to inflammation and protection after injury.