NON-PHARMACEUTICAL THERAPIES FOR PAIN MANAGEMENT
The development of novel, non-pharmaceutical therapies for pain management is a goal of military medical research. My research has played a major role in establishing the validity of the photonic specialty known as Photobiomodulation (PBM). Photobiomodulation therapy (PBMT) utilizes primarily red or near infrared (NIR) light to induce cellular changes producing beneficial clinical outcomes.
My laboratory has focused on central nervous system (CNS) and peripheral nervous system (PNS) injury and repair mechanisms and light tissue interactions. I am a recognized pioneer in the development of photonic therapies to non-invasively treat CNS and PNS injuries and accelerate wound healing. This research included characterization of the effects of light on tissues and cells at the molecular and functional levels, determination of depth of penetration of various wavelengths of light when applied to the skin, and optimization of dose. My research established the optimal near infrared (NIR) wavelengths for depth of penetration to the level of spinal cord and into the brain when light is applied to the skin. Further, we showed that light altered gene expression in many cell types including neurons and glia, and when delivered transcutaneously, improved recovery after spinal cord injury by altering the immune response and the secondary injury cascade.
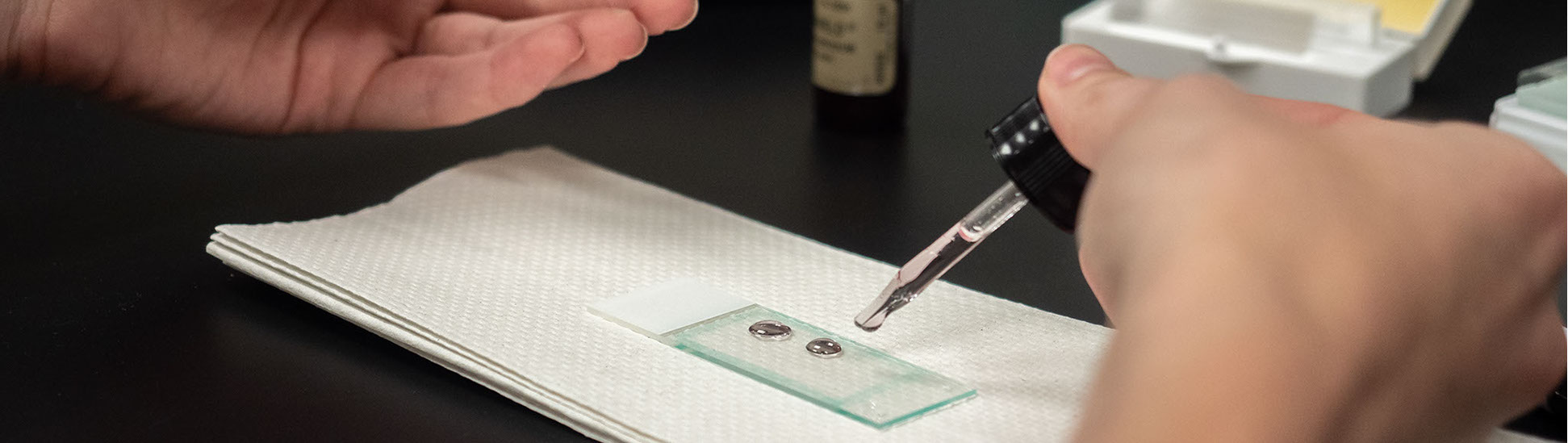
Recently, my research efforts have centered on the efficacy of Photobiomodulation Therapy (PBMT) for treatment of pain. We demonstrated that pain can be regulated with light by different mechanisms related to irradiance and time (dose). Using a spared nerve injury (SNI) preclinical model of neuropathic pain, we established that NIR PBMT effectively reduced mechanical hypersensitivity and modulated macrophage/microglial activation to an anti-inflammatory phenotype. Using in vivo and in vitro experimental models, we determined the mechanistic basis of PBMT for the treatment of pain using high irradiance, 810 nm wavelength light. Our results demonstrated a significant decrease in mitochondrial metabolism and the formation of varicosities and undulations in neurites of small and medium DRG neurons which represent the unmyelinated type C fibers and the lightly myelinated Aδ fibers related to pain, temperature, and light touch.
My laboratory is currently focusing on 5 funded projects:
1. Transforming Technology for the Warfighter: “Phase 1/Phase 2 Design and Testing of a Photobiomodulation Therapy Mobile Device for Pain Control”. The goal is to design, test, build and deliver a prototype mobile device for pain control. We are working closely with our industrial partner, Dr. Brian Pryor, B&W Tech on device development.
2. "Characterization of the Properties and Mechanisms of Photobiomodulation-Induced Axonal Block and Evaluation as a Treatment for Neuropathic Pain. The goal is to characterize aspects of PBM-induced axonal block (PAB) that are important for mechanistic understanding and translation as a clinical therapy. I am collaborating with my Co-PIs on this 5 year NIH project, Drs. Michael Moffitt and Michael Jenkins, Case Western Reserve University, Department of Biomedical Engineering.
3. Photomodulation Project 15: “Assessing User Application and Biological Effects of Commercially Available Photobiomodulation Devices in a Military Setting. This study will capture the current application of commercially available photobiomodulation devices in military populations, and assess the biological effects of applying those devices in a general wellness manner. My Co-PI on this project is Melissa Givens MD, MPH, Associate Professor, Department of Military and Emergency Medicine, USU.
4. "Efficacy of Light Therapy for Peripheral Neuropathies" The goal of this research is two-fold: to establish optimized dosing parameters for treatment of neuropathic pain and to establish optimized laser parameters for different near-infrared wavelengths and combination of wavelengths determined in vitro by mitochondrial functional analysis.
5. “Final-Stage Preclinical Development of a Long-Acting, Non-Opioid Peptidomimetic Drug for Chronic Pain” The objective of this proposal is to submit an IND for ASCT-83 for chronic neuropathic pain after establishing the route of administration, chemical manufacturing controls, determining the PK/ADME of ASCT-83, and assessing its safety to support first-in-human dosing.