THE PROBLEM
Infectious disease remains a leading cause of death in the world and bacterial infections account for a large proportion of these events. Furthermore, infectious disease significantly impacts military readiness and operations. Despite our best efforts, very few effective vaccines against bacterial pathogens have been developed, and we do not fully understand the process of human-bacterial interaction. Developing this understanding is complicated by the fact that many bacteria live a “Jekyll and Hyde” lifestyle where they can exist as a normal healthy component of the bacteria that colonize humans but then, upon some event, can cause severe disease that kills the host. Understanding more about the complex interplay that occurs during pathogenic interactions and how these interactions can lead to the development of various types of disease could help us develop ways to treat or prevent these deadly infections.
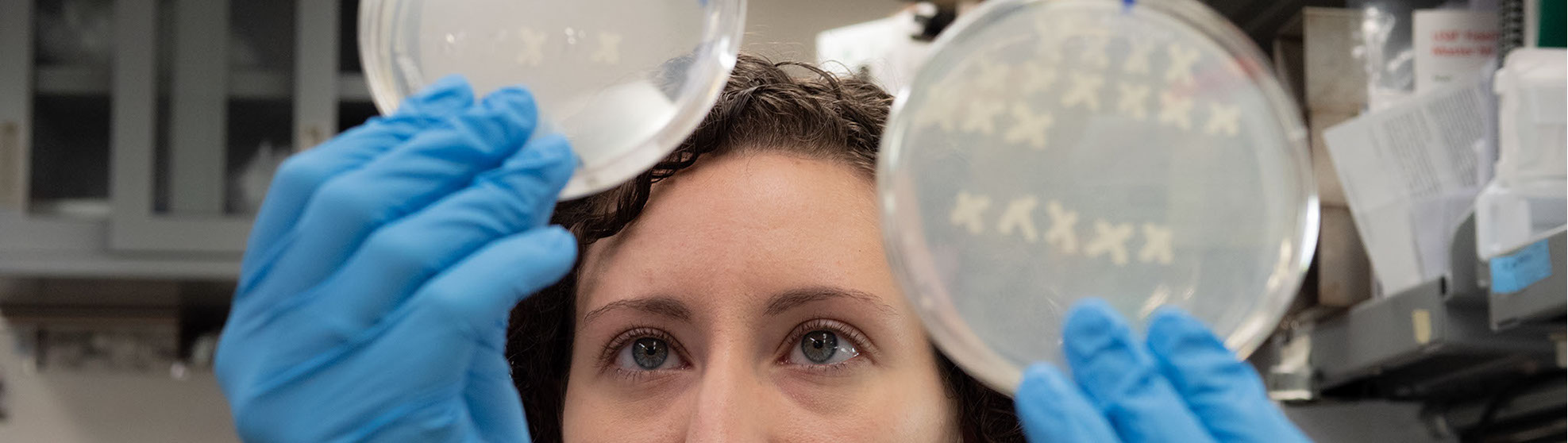
The Merrell lab focuses on the complex interplay that occurs during pathogenic interactions, and how these interactions can lead to the development of various types of disease. To increase the breadth of our findings, lab studies are currently focused on several bacterial pathogens: Helicobacter pylori, Staphylococcus aureus, and Acinetobacter baumannii. All of these bacteria have the ability to colonize humans without causing disease. However, each of them are also important human pathogens that result in significant morbidity and mortality in infected individuals.
OUR APPROACH
Ongoing studies are diverse and include: a) study of factors that allow H. pylori to colonize the human stomach and to induce gastric cancer/ulcers/intestinal metaplasia, b) H. pylori biofilm formation, c) microbiota associated with development of cancer, d) microbiota changes associated with S. aureus colonization and disease, e) S. aureus-mediated skin and soft tissue infections, f) mechanisms of resistance to antiseptics and resistance gene spread among S. aureus isolates, g) polymicrobial interactions as a means to inhibit S. aureus, and h) copper resistance in A. baumannii. Laboratory approaches include bacterial genetics, molecular microbiology, epidemiology, genomics, and biochemistry.
"Understanding more about the complex interplay that occurs during pathogenic interactions and how these interactions can lead to the development of various types of disease could help us develop ways to treat or prevent these deadly infections."